MORE OPTIONS TO FIND YOUR MATCH.
At LBE, we believe when we help expand the number of donor lungs available, we help make more transplants happen. That’s why we are constantly innovating to make more donor lungs available so that more patients may receive a transplant.
01 | Why EVLP?
The difficult journey of end-stage lung disease
An end-stage organ disease diagnosis can feel insurmountable.
For those living with chronic lung diseases such as Idiopathic Pulmonary Fibrosis (IPF), Pulmonary Hypertension (PH), Cystic Fibrosis (CF) and Chronic Obstructive Pulmonary Disease (COPD), the only path forward is often lung transplant. Yet, the road to transplant has many obstacles, the largest being the availability of a suitable donor lung. Lungs not only must be a match, they must be healthy enough to be transplanted.
Only 25% of donor lungs are used for transplant.1 Every year, this lack of viable donor lungs is the end to many patient journeys.
ONLY 25% of available donor lungs are used for transplantation.
75% of donor lungs are rejected1
Expanding the pool of donor lungs with EVLP
Ex vivo lung perfusion (EVLP) holds promise for improved preservation and additional assessment to evaluate organs before transplant. This technology has had an important impact on transplant medicine in the U.S. (and globally), expanding the donor pool by allowing surgeons to assess and successfully transplant organs that once would have gone unused.
IMPORTANT SAFETY INFORMATION FOR XVIVO PERFUSION SYSTEM (XPS™) WITH STEEN SOLUTION™ PERFUSATE - P180014
Warnings and Precautions
General Warnings
The safety and effectiveness of the XPS™ System with STEEN Solution™ Perfusate device were not evaluated with ideal criteria donor lungs.
Risk for Contamination and Mechanical Trauma
The degree of organ manipulation required for airway and vascular cannulation carries the potential for contamination and mechanical trauma of the donor lungs. Even though not contraindicated, it is not recommended to use an organ with evident signs of mechanical trauma or major contamination.
Please see full Important Safety Information by clicking the button below
02 | WHAT IS EVLP?
Understanding EVLP
EVLP, (ex vivo lung perfusion) uses FDA-approved medical technology that evaluates donor lungs, giving them a second chance at transplantation.
EVLP allows physicians to monitor and evaluate the lungs prior to transplant in order to provide a clearer picture of lung health.
how does evlp help?
EVLP gives the transplant team a second look to decide whether lungs can be used for transplant.
EVLP allows the organ transplant team to prolong the time that lungs are outside the donor body so they can be evaluated.
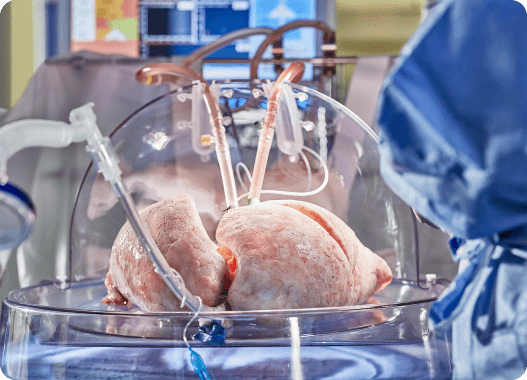
The EVLP system attempts to mimic the functionality of the body. The donor lungs are attached to a ventilator, pump, and filters. The lungs are maintained at normal body temperature and perfused.
EVLP makes it possible for organs to be transported over greater distances. This may help hospitals in procuring lungs from donors that are farther away.
LUNG BIOENGINEERING UTILIZES THE FIRST FDA-APPROVED EVLP TECHNOLOGY ON THE MARKET.
We also offer the only service in the United States that houses all EVLP tools and resources in one place—making it easier for transplant centers to incorporate EVLP technology into their program.
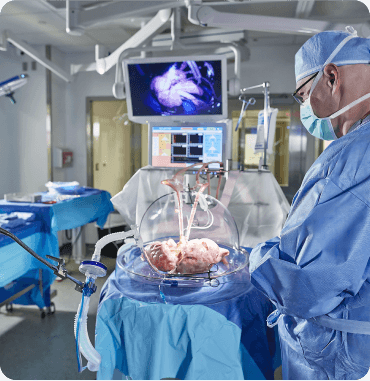
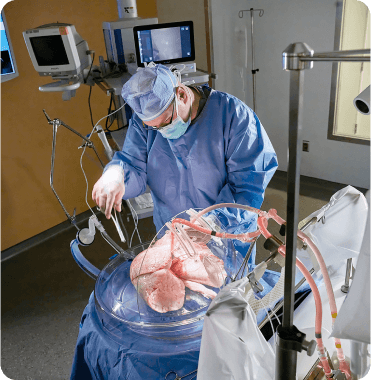
How EVLP works
EVLP is a tool used to evaluate a donor lung for transplant. The lung is ventilated, warmed and assessed outside of the human body to help determine it's function and suitability for transplant. After EVLP, if the lung is deemed suitable for transplant by a transplant physician, it will be sent to the organ transplant center and may then be transplanted into a waiting patient.
EVLP creates an environment for gathering data from potentially transplantable lungs
The EVLP system is designed to provide the lungs with an environment similar to the inside of the body. During EVLP, a team of Specialists warms the lungs to body temperature while they undergo perfusion, a process that helps to drive fluid flow into capillaries. The lungs are then ventilated and tested for medical experts to observe their function and determine whether or not they are suitable for transplant.
03 | HOW CAN I ACCESS EVLP?
Lung Bioengineering teams up with your Transplant Center


Lung Bioengineering (LBE) is an EVLP service provider with two dedicated EVLP centers in Silver Spring, Maryland and Jacksonville, Florida. These centers work with organ transplant centers across the United States to minimize any challenges that could arise in the process of keeping a lung healthy from the time it is donated through its transplant.
Our EVLP teams are staffed by experts available 24/7/ 365 to work in lockstep with physicians throughout the transplant journey.
04 | IS EVLP SAFE?
Yes, EVLP is Safe.
EVLP has been used in clinical practice for 10 years and has safely increased lung transplantation activity throughout that time. Several studies demonstrate that organ transplant patients who receive donor lungs treated with EVLP experience similar outcomes to those receiving standard donor lungs.
If you have been diagnosed with an end-stage lung disease and are considering a lung transplant, talk with your doctor about whether EVLP might be possible through your transplant center.
Contact Us
To learn more about Lung Bioengineering, and how to get started, please fill out the form.
References:
- Reul RM, Loor G, Garcha PS, Goss JA, Rana AA. Allograft discard risk index for lung transplantation. J Heart Lung Transplant. 2021 Dec;40(12):1658-1667. doi: 10.1016/j.healun.2021.08.017. Epub 2021 Sep 9. PMID: 34836606. Back to content
- Ex Vivo Lung Perfusion: A Key Tool for Translational Science in the Lungs. Tane S., Noda K., Shigemura N. (2017) Chest, 151 (6), pp. 1220-1228. Back to content